A recently published paper describing free-roaming cats as “a significant public health threat” fails to deliver convincing evidence. In fact, the very work the authors cite undermines, time and time again, their claims.
“Domestic cats are a potential source of numerous infectious disease agents,” write Rick Gerhold and David Jessup, in their paper, “Zoonotic Diseases Associated with Free-Roaming Cats,” published online in July by the journal Zoonoses Public Health (and to be included in an upcoming print edition).
“However, many of these diseases are controlled in cats belonging to responsible owners through routine veterinary care, proper vaccination regimens and parasite chemotherapy. Free-roaming cats often lack the necessary preventative care to control these diseases and consequently pose a potential health threat to other domestic animals, wildlife and humans.” [1]
Just how much of a threat do these cats pose?
Gerhold and Jessup would have us believe that the risks are high and the consequences dire. A careful reading of their paper, however, reveals the authors’ tendency to cherry-pick some studies and misrepresent others. And, occasionally, simply get their facts wrong.*
All of which raises serious questions about Gerhold and Jessup’s case against free-roaming cats.
This should come as no surprise, though. This is the same David Jessup, after all, who authored the 2004 paper, “The welfare of feral cats and wildlife,” in which he argued that “TNR really stands for trap, neuter, and re-abandon” and that it “may be illegal” (without citing any legal cases—there being none to cite). And warned that “more than 90,000 cats did not receive rabies vaccinations” as part of 1999–2001 Maddie’s Fund project in California (failing to mention that rabies in cats is virtually non-existent in the state).
And Jessup and Gerhold were among “22 experts in wildlife and veterinary public health from around the United States” to co-author a June 2011 letter to Maureen Lichtveld, Chair, Science Board, American Public Health Association), “oppos[ing]… in the strongest possible terms” the APHA’s potential endorsement of TNR. Among their objections: “TNR legislation routinely interferes with the ability of public health professionals to abate public health risk (e.g., presence of fleas and feces associated with feral cat colonies).” [2] (Not surprisingly, many of the complaints included in the letter to Lichtveld are repeated in “Zoonotic Diseases Associated with Free-Roaming Cats.”)
To be clear: I don’t object to scientists shaping policy; on the contrary, I think we’d all be better off if there were more of it. But only if the scientists involved are able to set aside (or, failing that, at least acknowledge) their biases and produce work that can withstand the scrutiny not of their peers (who, as we’ll see, are either unable or unwilling to provide the necessary oversight), but of their critics.
Rabies
Gerhold and Jessup don’t devote much attention to cases in which humans contract rabies from cats, probably because there are so few—not that the authors acknowledge even that basic fact.
Rabies Cases in Humans
Of the 49 rabies cases reported in humans since 1995, 10 were the result of dog bites that occurred outside of the U.S.; the remainder were traced either to wildlife or were of unknown origins. [3] Since 1960, only two cases of human rabies have been attributed to cats. [4] As I pointed in a post this past August, you’ve got a much better chance of being killed by lightning—not just struck, but killed by lightning.
Data collected by the National Oceanic and Atmospheric Administration show that between 1959 and 2011, 3,947 people in the U.S. were killed by lightning. [5] That’s roughly 75 deaths annually due to lightning strikes. Compared to just two from rabies related to cats over the past 52 years (and, for the record: in one of those cases, the woman was bitten while traveling in Guatemala and then treated in the U.S. [6]).
Post-exposure Prophylaxis
“Individuals exposed to potentially rabid animals are administered post-exposure prophylaxis,” explain Gerhold and Jessup, “and cat exposures account for approximately one-third of all PEP recipients.” And, claim the authors, “the actual cases of rabies exposure in humans owing to cats are likely underestimated.” [1]
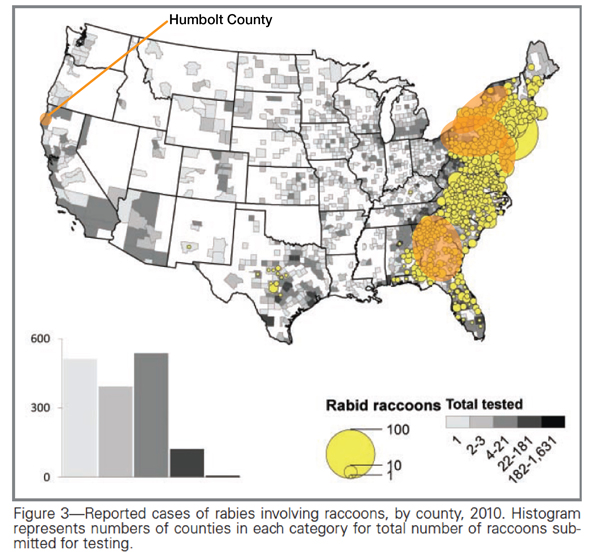
I’ve been unable to locate any national figures for PEP from the Centers for Disease Control and Prevention (CDC), and the examples the authors cite (shown in orange on the map below, adapted from [7]) nearly all come from the mid-Atlantic and Southeast, where reports of raccoon rabies have risen sharply since the mid-1970s and “the importation of rabid raccoons from Florida by hunters.” [8–10] (The one exception involves eight-year-old Precious Reynolds of Humbolt County, California. I’ll come back to this case shortly.)
And where raccoon cases increase, cat cases tend to follow. In the western part of the country, by contrast, rabid cats (and rabid raccoons) are, as I mentioned previously, nearly unheard of.
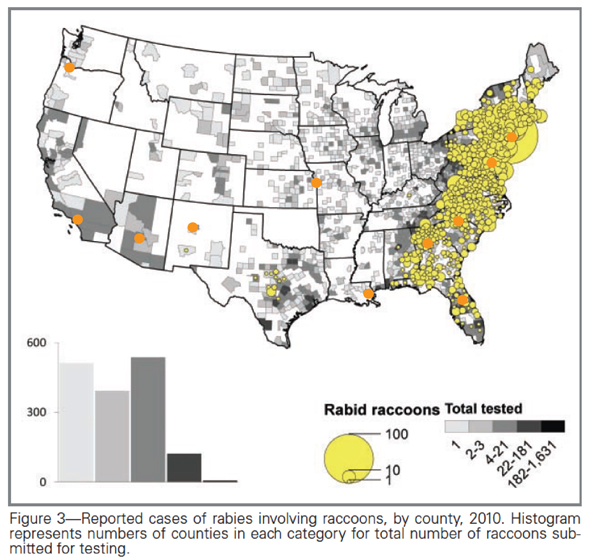
A more representative perspective is provided by a study of “11 geographically diverse university-affiliated, urban emergency departments” (shown in the map below), which found that of 2,030 patients enrolled, 1,635 exposures (81 percent) were attributed to dogs, and 268 (13 percent) to cats. [11] This same study found that PEP was applied unnecessarily in about 40 percent of the cases documented. Other research has documented similar instances of PEP overuse [12–15], and suggested that such costly policy failures can be exacerbated by “media hysteria.” [15]
Gerhold and Jessup (and ABC) go on to argue that “human exposure to rabies is largely associated with free-roaming cats because of people being more likely to come in contact with cats, large free-roaming cat populations, and lack of stringent rabies vaccination programmes.” [1] In fact, a 2012 nationwide survey of “feral cats groups” conducted by Alley Cat Rescue revealed that 96 percent of them provide rabies vaccinations as part of their TNR programs. [16] And TNR not only reduces the risk of transmission from domestic animals to humans, but also serves as a barrier between wildlife and humans. Recalling one of his early-1990s TNR projects, Merritt Clifton, editor of Animal People , says it “proved the efficacy… to keep raccoon rabies from spreading among feral cats at eight sites in Connecticut.” [17]
Of course, many of these cats rarely come into contact with humans to begin with. A 1993–94 study of four upstate New York counties found that 79 percent of 202 PEP cases related to cats were the result of provocation, “characterized by intentional, human-initiated interaction with a suspect rabid animal.” [12]
Cost of PEP
“Post-exposure prophylaxis regimen generally costs $5,000–8,000 for each individual,” write Gerhold and Jessup, “which is mostly borne by public health agencies.” [1] In fact, the very source the authors cite puts the “average terrestrial rabies-associated PEP cost” at “$941.06, with a range of $440.21 to $1,884.97,” based on three-year study of five upstate New York counties. [14] (Terrestrial rabies, in this case, refers to “primarily dogs, cats, raccoons, and skunks,” which made up “70 of the specimens submitted for testing.” Bats made up the other 30 percent. [14])
“The average per capita cost for terrestrial rabies including PEPs, specimen preparation/shipment, and pet vaccination clinics was $0.32, with a range of $0.10 to $0.77.” [14] That’s right: less than a buck per county resident.
The cost figures for upstate New York correspond quite well with those from the CDC: “a course of rabies immune globulin and five doses of vaccine given over a 4-week period typically exceeds $1,000.” [18] Of course, Gerhold and Jessup aren’t the first to be so wildly off the mark. In their brochure Rabies in Humans and Wildlife, The Wildlife Society claims PEP “can cost $7,000 or more.” [19]
This rather monumental error reflects poorly not only on the authors—when your “facts” are even less factual than TWS’s “facts,” it’s probably time to turn in your credentials—but also on the peer-review process so often defended by TNR opponents. If the reviewers involved (1) weren’t familiar enough with the topic to recognize the error and/or (2) were unwilling to quickly check with the CDC website, they simply shouldn’t be reviewing such work.
Precious Reynolds
In 2011, an eight-year-old Humbolt County, CA, girl contracted rabies and made headlines nationwide, as she was just “the third person in recent U.S. history to recover from rabies without getting the rabies vaccine.” [20] Describing Precious Reynolds’ case, Gerhold and Jessup write:
“A recent case of rabies in an 8-year old girl from California in 2010 disclosed that the patient had multiple cat bites from free-roaming cat colonies near her house (Blanton et al., 2011). Although rabies RNA was unable to be collected for molecular typing, the epidemiological data highly suggest that the girl was exposed by a rabid free-roaming cat (CDC MMWR, 2012).” [1]
The fact that the authors got the year wrong is only the beginning. Here again, we’re not getting the whole story. They fail to acknowledge, for example, how cautious Blanton et al. were in their report on the case:
“She… had multiple cat bites from at least two cats in a feral cat population residing near her school. While the presence of bats was noted around the farm, no infestation was noted in the household, and no contact with a bat was reported. The lack of any isolated rabies virus in this case makes further analysis of exposure route speculative.” [7, emphasis mine]
And the CDC report cited by Gerhold and Jessup provides additional context the authors ignore—including the “news” that there were no bites at all:
“The patient confirmed having contact with free-roaming, unvaccinated cats at her school on several occasions. She was scratched by two different cats approximately nine weeks and four weeks before illness onset but reported no bites. Local public health officials implemented a program to collect and identify cats at the school. The first cat was observed to be healthy, but a reliable description of the second cat was not available. All other cats collected at the school remained healthy under observation.” [4]
Q: If there’s a compelling case to be made regarding the rabies threat posed by free-roaming cats, why do Gerhold and Jessup go out of their way to misrepresent the research?
A: There’s not a compelling case to be made regarding the rabies threat posed by free-roaming cats.
Plague
“Approximately 8 percent of plague cases in the United States are associated with transmission from cats,” write Gerhold and Jessup. “Cats frequently develop the pneumonic form of plague, which is considerably more infectious to humans in close contact, and results in rapidly progressive and frequently fatal disease.” [1] But the authors fail to mention the number of cases associated with cats: 23 from 1977 through 1998, according to the study the authors cite as support. And only five of those were pneumonic plague. [21]
Over that same 23-year period, five people died of plague contracted through contact with a cat; only two of those cases were pneumonic plague. And the fatal cases were “associated with misdiagnosis or delays in seeking treatment, which resulted in overwhelming infection and various manifestations of the systemic inflammatory response syndrome.” [21]
By comparison, about 1,725 people in the U.S. were killed by lightning between 1977 and 1998.
Toxoplasmosis
Toxoplasma gondii is a parasite “that infects most, if not all, species of birds and mammals.” [22] Felids—the domestic cat as well as the “big cats” (e.g., bobcats, cougars, etc.)—are the only known definitive hosts; the parasite reproduces sexually in a cat’s small intestine, and potentially infectious spores are then passed in the cat’s feces. (This process, called “shedding oocysts,” typically occurs only once during a cat’s lifetime, and lasts only about a week. [23])
Cats become infected when they consume an intermediate host infected with T. gondii (i.e., containing tissue cysts). Humans become infected by ingesting “oocyst-contaminated soil and water, from tissue cysts in undercooked meat, by transplantation, blood transfusion, laboratory accidents, or congenitally.” [22]
As Gerhold and Jessup point out, recently published research suggests that the risk of infection from oocysts may be greater than previously thought. [24] Even so, drawing a direct connection to domestic cats seems premature. Indeed, a careful reading of the work the authors cite reveals that three of 103 such infections were actually the result of contaminated water linked to cougars in the area of a local reservoir. [25]
With every new study of T. gondii comes a host of new questions. Why, for example, are outbreaks caused by contaminated drinking water [25] not more common, given the number of free-roaming cats in the environment? Or other types of outbreaks linked to environmental contamination? In 1997, 37 people were diagnosed with toxoplasmosis after visiting a riding stable in Atlanta, GA, and a subsequent investigation implicated cats on or near the property. [26] (Nine of 11 submitted for testing were recently attributed to oocysts, and included among the 103 infections mentioned previously.) But there’s nothing unusual about keeping cats in horse stables and barns. Why, then, are such occurrences so uncommon?
Clearly, there’s a great deal we don’t yet know about this common parasite. It’s telling, though, that some of the scientists closest to the research don’t share the alarmist views of TNR opponents.
Jaroslav Flegr, whose pioneering research was the focus of a feature article in the March 2012 issue of The Atlantic, for example, shares his family home (Flegr is a husband and father of two young children) with two indoor-outdoor cats. [27] Robert Yolken, an infectious disease expert at Johns Hopkins University, also a guardian of two cats, told NPR, simply: “the benefits outweigh the risks.” [28]
Others, investigating the congenital transmission of toxoplasmosis (i.e., from mother to fetus), are calling for the screening of pregnant women (standard practice in France) and the development of vaccines. [29–30]
If these researchers aren’t demanding the roundup of outdoor cats in the name of public safety, what justification do TNR opponents have?
Baylisascaris procyonis
Gerhold and Jessup argue that the feeding stations commonly used by colony caregivers attract raccoons, which “harbour an intestinal nematode parasite, Baylisascaris procyonis (i.e., raccoon roundworm), that has caused morbidity and mortality in humans, especially children.” [1] But once again, these two overstate the threat. Indeed, as the authors of one of the studies cited by Gerhold and Jessup explain, “human infection with Baylisascaris is probably common.”
“Many more people will contract low-level infections than heavy infections, and unless the larvae migrate to the eye or brain in sufficient numbers, these individuals will not develop clinically significant disease… most human infections with Baylisascaris are probably asymptomatic.” [31]
Gerhold and Jessup go on to imply that a connection between TNR and the distribution of B. procyonis: “The finding of B. procyonis in raccoons only near urban areas in Georgia is of particular interest given that managed free-roaming cat colonies are likely to be found in urban and suburban settings.” [1] Here, too, the very study they cite as support provides some additional information Gerhold and Jessup ignore:
“Urbanized raccoons are more likely to forage in refuse and other human-provided food sources that would decrease the chances of a raccoon ingesting B. procyonis–infected paratenic hosts… urbanized raccoons have been shown to have smaller home ranges, which limit contact and foraging in potentially contaminated areas.” [32]
Suddenly those feeding stations don’t seem like such a public health threat. In fact, if the concern is really B. procyonis, then we need to provide raccoons with more food sources, not fewer.
Threats to Wildlife and Cats
The threats posed by free-roaming cats are, according to Gerhold and Jessup, not limited to humans. Wildlife—even other domestic cats—are at risk of disease. As with so many of Gerhold and Jessup’s claims, though, drilling down into the work they cite as support often reveals research findings that—guess what?—provide no such support. (Perhaps the authors assumed nobody would bother checking.)
Feline Immunodeficiency Virus and Feline Leukemia Virus
If the evidence throughout Gerhold and Jessup’s paper is less than convincing, their section on FIV and FeLV is downright bizarre.
“In a prospective study of FeLV and feline immunodeficiency virus (FIV) in Canada, the authors noted that 6 percent (n = 14) of free-roaming cats were FeLV seropositive, whereas only 2 percent (n = 4) of owned cats were FeLV seropositive (Little, 2011). The risk of being seropositive for either virus was most frequently associated with being free-roaming, followed by having access to outdoors.” [1]
In her 2011 paper, veterinarian Susan Little, “one of only four board-certified feline specialists in Canada,” according to the Bytown Cat Hospital website, summarizes eight studies of “FeLV and FIV seroprevalence for Canadian cats.” [33] However, none seems to correspond to Gerhold and Jessup’s description. Across the eight studies Little cites, FeLV infection rates vary from 2.5 to 7.7 percent. (In most cases, no breakdown is provided to distinguish between free-roaming and owned cats.)
Little also provides evidence demonstrating the benefits of TNR: “FeLV seropositivity was highest in intact females (7.3 percent) and intact males (7.1 percent) and FIV seropositivity was highest in intact males (7.4 percent).” [33, emphasis mine] And, citing her 2005 Canadian Veterinary Journal paper in which Little documented “seroprevalence in 246 cats from three demographic populations in Ottawa, Ontario.” (Specifically: “74 unowned urban strays… as well as 20 cats from a small feral cat colony, and 152 client-owned cats.” [34])
“Seroprevalence of FIV was highest in urban stray cats (23 percent) and lower in client-owned cats (5.9 percent) and in a feral cat colony (5 percent). The same groups of cats had 6.7, 2.6 and 0 percent seroprevalence of FeLV, respectively.” [33]
Interestingly, the one FIV-positive colony cat observed in this study “probably did not originate in the colony,” according to Little, “for it was clearly a socialized cat, whereas almost all other members of the group were truly feral.”
“It may be that this single FIV-positive male had migrated into the colony recently from another area of the city. This cat was not released back into the colony but placed in a foster home.” [34]
Little’s findings correspond with those of Lee et al., whose study of 1,876 colony cats revealed a 4.3 percent rate of FeLV prevalence, and a 3.5 percent rate of FIV seroprevalence—“similar to infection rates reported for owned cats.” [35]
Florida Panthers
“Genetic analysis of the FeLV virus associated with mortality in five Florida panthers,” explain Gerhold and Jessup, “indicated that the virus envelope sequence was nearly identical indicating the source or [sic] the infection was likely from a single domestic cat.” [1] What the authors don’t explain is that, in response, “the Florida Department of Fisheries and Wildlife began a widespread vaccination program of Florida panthers.” [36] And as a result, “there have been no new cases since July 2004.” [37]
Once again, these additional “details” come from the very studies Gerhold and Jessup cite.
• • •
“While citizens who are concerned about the perceived improved welfare of cats in TNR programmes may be very vocal in their support of free-roaming cat populations,” warn Gerhold and Jessup, “local, county and state legislative and medical officials need to understand the economic and public health threats associated with various policies and laws associated with free-roaming cat populations.” [1] If the authors’ intention was to in some way add to this understanding, they clearly fell far short. Gerhold and Jessup argue: “Further resources are needed to educate the public, the medical community and public health officials about the zoonotic disease potential associated with free-roaming cats.” [1]
But it’s not a matter of additional resources as much as it is different resources. Provided by—not to put too fine a point on it—different researchers.
* And then there are the dubious claims that lack any supporting evidence whatsoever—for example: “Diminished resources and willingness to collect free-roaming animals have led to increasing numbers of free-roaming animals.”
Literature Cited
1. Gerhold, R.W. and Jessup, D.A., “Zoonotic Diseases Associated with Free-Roaming Cats.” Zoonoses Public Health. 2012. http://www.ncbi.nlm.nih.gov/pubmed/22830565
2. Barrows, P.L., et al., Proposal to designate Trap-Neuter-Vaccinate-Return as preferred management scheme for feral cats (letter to Maureen Lichtveld, Chair, Science Board, American Public Health Association). 2011.
3. CDC, Human Rabies. 2012, Centers for Disease Control and Prevention: Atlanta (GA). http://www.cdc.gov/rabies/location/usa/surveillance/human_rabies.html
4. CDC, “Recovery of a Patient from Clinical Rabies—California, 2011.” Morbidity and Mortality Weekly Report. 2012. 61(4): p. 61–64. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6104a1.htm
5. Holle, R., Lightning Fatalities by State, 1959–2011. 2012, Vaisala: Tucson, AZ. http://www.lightningsafety.noaa.gov/stats/59-11_fatalities_rates.pdf
6. Ross, E. and Armentrout, S.A., “Myocarditis Associated with Rabies—Report of a Case.” New England Journal of Medicine. 1962. 266(21): p. 1087–1089. http://www.nejm.org/doi/full/10.1056/NEJM196205242662105
7. Blanton, J.D., et al., “Rabies surveillance in the United States during 2010.” Journal of the American Veterinary Medical Association. 2011. 239(6): p. 773–783. http://www.ncbi.nlm.nih.gov/pubmed/21916759
http://avmajournals.avma.org/doi/pdf/10.2460/javma.239.6.773
8. Jenkins, S.R. and Winkler, W.G., “Descriptive Epidemiology from an Epizootic of Raccoon Rabies in the Middle Atlantic States, 1982–1983.” American Journal of Epidemiology. 1987. 126(3): p. 429–437. http://aje.oxfordjournals.org/content/126/3/429.abstract
9. Curtis, A., “Using a Spatial Filter and a Geographic Information System to Improve Rabies Surveillance Data.” Emerging Infectious Diseases. 1999. 5(5): p. 603–606. wwwnc.cdc.gov/eid/article/5/5/pdfs/99-0501.pdf
10. McCoy, J. (2012, May 24). Researches closer to eliminating raccoon rabies. The Charleston Gazette, from http://wvgazette.com/Outdoors/201205190101
11. Moran, G.J., et al., “Appropriateness of rabies postexposure prophylaxis treatment for animal exposures. Emergency ID Net Study Group.” Journal of the American Medical Association. 2000. 284(8): p. 1001–1007.
12. Wyatt, J.D., et al., “Human rabies postexposure prophylaxis during a raccoon rabies epizootic in New York, 1993 and 1994.” Emerging Infectious Diseases. 1999. 5(3): p. 415–423. http://www.ncbi.nlm.nih.gov/pubmed/10341178
13. Krebs, J.W., Long-Marin, S.C., and Childs, J.E., “Causes, costs, and estimates of rabies postexposure prophylaxis treatments in the United States.” Journal of Public Health Management and Practice. 1998. 4(5): p. 56–62. http://www.ncbi.nlm.nih.gov/pubmed/10187067
14. Recuenco, S., Cherry, B., and Eidson, M., “Potential cost savings with terrestrial rabies control.” BMC Public Health. 2007. 7(1). http://www.biomedcentral.com/1471-2458/7/47
15. Noah, D.L., et al., “Mass human exposure to rabies in New Hampshire: exposures, treatment, and cost.” American Journal of Public Health. 1996. 86(8): p. 1149–51. http://www.ncbi.nlm.nih.gov/pubmed/8712277
16. Alley Cat Rescue (2012) Alley Cat Rescue’s National Feral Cat Survey. PR Newswire http://www.prnewswire.com/news-releases/alley-cat-rescues-national-feral-cat-survey-157263395.html
17. Clifton, M. (2010). How to introduce neuter/return & make it work. Animal People, pp. 3–4, from http://www.animalpeoplenews.org/10/4/April10.htm
18. CDC (2011) Cost of Rabies Prevention. http://www.cdc.gov/rabies/location/usa/cost.html Accessed September 18, 2012.
19. TWS, Rabies in Humans and Wildlife. 2011, The Wildlife Society: Bethesda, MD. joomla.wildlife.org/documents/cats_rabies.pdf
20. Magagnini, S. (2011, June 13). Health officials still questioning how girl, 8, contracted rabies. Sacramento Bee, from http://www.sacbee.com/2011/06/13/3698009/health-officials-still-questioning.html
21. Gage, K.L., et al., “Cases of Cat-Associated Human Plague in the Western US, 1977–1998.” Clinical Infectious Diseases. 2000. 30(6): p. 893–900. http://cid.oxfordjournals.org/content/30/6/893.abstract
22. Elmore, S.A., et al., “Toxoplasma gondii: epidemiology, feline clinical aspects, and prevention.” Trends in Parasitology. 2010. 26(4): p. 190–196. http://www.sciencedirect.com/science/article/B6W7G-4YHFWNM-1/2/2a468a936eb06649fde0463deae4e92f
23. Dubey, J.P. and Jones, J.L., “Toxoplasma gondii infection in humans and animals in the United States.” International Journal for Parasitology. 2008. 38(11): p. 1257–1278. http://www.sciencedirect.com/science/article/B6T7F-4S85DPK-1/2/2a1f9e590e7c7ec35d1072e06b2fa99d
24. Hill, D., et al., “Identification of a Sporozoite-Specific Antigen from Toxoplasma gondii.” Journal of Parasitology. 2011. 97(2): p. 328–337. http://dx.doi.org/10.1645/GE-2782.1
25. Aramini, J.J., Stephen, C., and Dubey, J.P., “Toxoplasma gondii in Vancouver Island Cougars (Felis concolor vancouverensis): Serology and Oocyst Shedding.” The Journal of Parasitology. 1998. 84(2): p. 438–440. http://www.jstor.org/stable/3284508
26. Teutsch, S.M., et al., “Epidemic toxoplasmosis associated with infected cats.” New England Journal of Medicine. 1979. 300(13): p. 695–699. http://www.ncbi.nlm.nih.gov/pubmed/763300
27. McAuliffe, K., “How Your Cat Is Making You Crazy.” The Atlantic. 2012. March. http://www.theatlantic.com/magazine/print/2012/03/how-your-cat-is-making-you-crazy/8873/
28. Hamilton, J. (2012) A Parasite Carried By Cats Could Increase Suicide Risk. Shots (NPR Health BLog_ http://www.npr.org/blogs/health/2012/07/02/156142214/a-parasite-carried-by-cats-could-hurt-humans-sanity Accessed July 3, 2012.
29. Boyer, K., et al., “Unrecognized Ingestion of Toxoplasma gondii Oocysts Leads to Congenital Toxoplasmosis and Causes Epidemics in North America.” Clinical Infectious Diseases. 2011. 53(11): p. 1081–1089. http://cid.oxfordjournals.org/content/53/11/1081.abstract
30. Linn, E.S., “Prenatal Toxoplasma gondii.” Clinical Infectious Diseases. 2011. 53(11): p. 1090–1091. http://cid.oxfordjournals.org/content/53/11/1090.short
31. Kazacos, K.R., Baylisascaris procyonis and Related Species, in Parasitic diseases of wild mammals, W.M. Samuel and M.J. Pybus, Editors. 2001, Iowa State University Press: Ames. p. viii, 559 p.
32. Blizzard, E.L., et al., “Distribution, Prevalence, and Genetic Characterization of Baylisascaris procyonis in Selected Areas of Georgia.” Journal of Parasitology. 2010. 96(6): p. 1128–1133. http://dx.doi.org/10.1645/GE-2518.1
33. Little, S., “A review of feline leukemia virus and feline immunodeficiency virus seroprevalence in cats in Canada.” Veterinary Immunology and Immunopathology. 2011. 143(3-4): p. 243–245. http://www.ncbi.nlm.nih.gov/pubmed/21757241
34. Little, S.E., “Feline immunodeficiency virus testing in stray, feral, and client-owned cats of Ottawa.” Canadian Veterinary Journal. 2005. 46(10): p. 898–901. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1255591/
35. Lee, I.T., et al., “Prevalence of feline leukemia virus infection and serum antibodies against feline immunodeficiency virus in unowned free-roaming cats.” Journal of the American Veterinary Medical Association. 2002. 220(5): p. 620-622. http://avmajournals.avma.org/doi/abs/10.2460/javma.2002.220.620
36. Brown, M.A., et al., “Genetic Characterization of Feline Leukemia Virus from Florida Panthers.” Emerging Infectious Diseases. 2008. 14(2): p. 252–259.
37. Cunningham, M.W., et al., “Epizootiology and management of feline leukemia virus in the Florida puma.” Journal of Wildlife Diseases. 2008. 44(3): p. 537–552. http://www.ncbi.nlm.nih.gov/pubmed/18689639